Sleep and PTSD Management Restful Recovery
Sleep and PTSD management are intrinsically linked. Post-traumatic stress disorder significantly disrupts sleep patterns, leading to a vicious cycle where poor sleep exacerbates PTSD symptoms, and vice-versa. This exploration delves into the complex relationship between sleep and PTSD, examining the various sleep disturbances common in PTSD sufferers, the physiological mechanisms underlying these disruptions, and the impact of sleep deprivation on PTSD symptom severity.
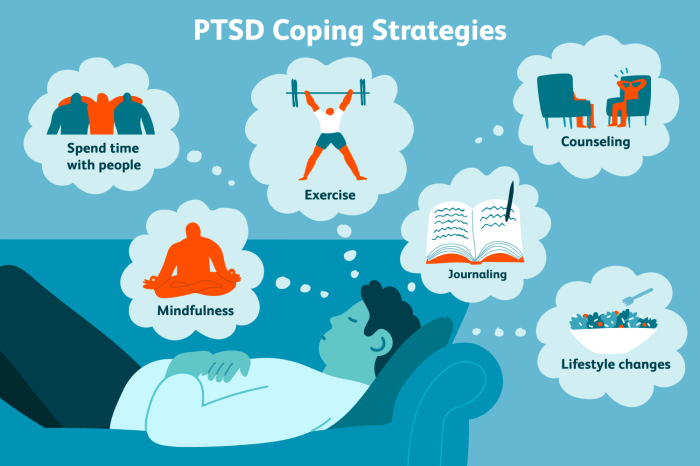
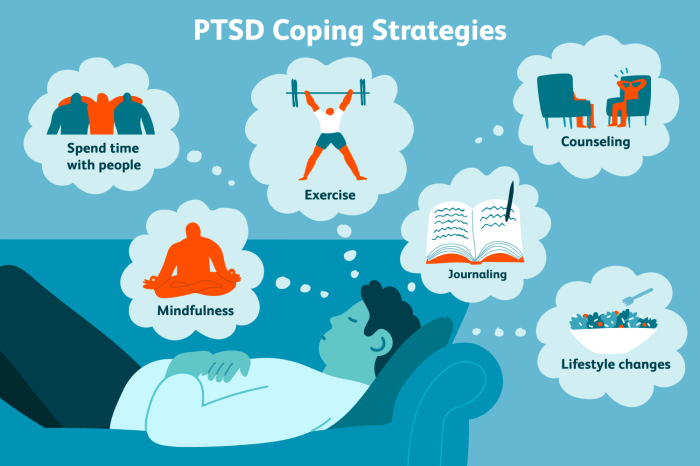
We’ll also investigate effective strategies for improving sleep quality, encompassing sleep hygiene practices, therapeutic interventions, and stress management techniques.
Understanding the multifaceted nature of this relationship is crucial for effective PTSD treatment. By addressing sleep problems, we can significantly improve overall mental health and enhance the efficacy of other PTSD therapies. This comprehensive overview will equip readers with a deeper understanding of the problem and provide actionable strategies for better sleep and improved well-being.
The Impact of PTSD on Sleep
Post-traumatic stress disorder (PTSD) significantly impacts sleep, leading to a range of disturbances that exacerbate existing symptoms and hinder recovery. The disruption of sleep is not merely a consequence of PTSD; it is a crucial factor contributing to the maintenance and worsening of the disorder’s debilitating effects. Understanding this complex interplay is essential for developing effective treatment strategies.
Common Sleep Disturbances in PTSD
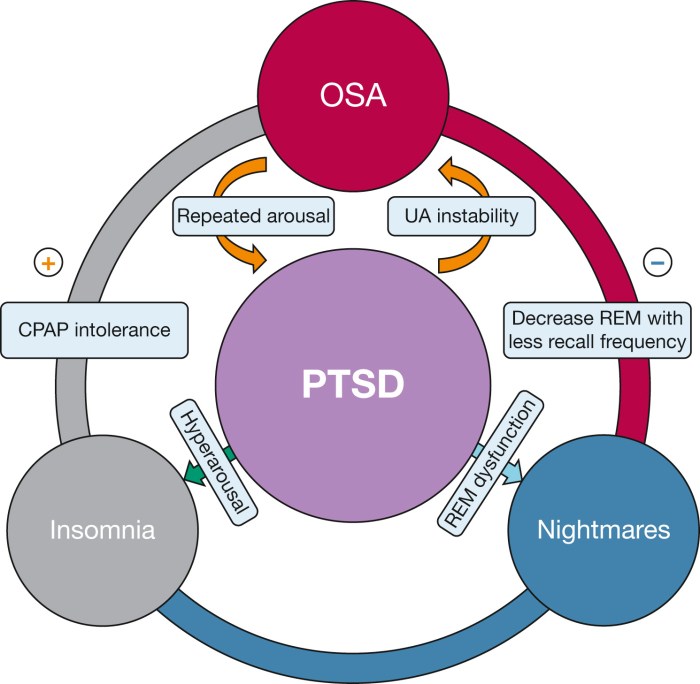
Individuals with PTSD frequently experience a variety of sleep problems. These can include insomnia, characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep. Nightmares, often vivid and related to the traumatic event, are another common feature. Sleepwalking and sleep terrors, typically associated with deep sleep, can also occur. Furthermore, individuals may experience hyperarousal, characterized by difficulty relaxing and falling asleep, and frequent awakenings.
These sleep disturbances significantly impact the quality of life for those affected.
Physiological Mechanisms Linking PTSD and Sleep Disorders
The link between PTSD and sleep disorders is multifaceted and involves several physiological mechanisms. The amygdala, a brain region crucial for processing fear and emotions, is hyperactive in individuals with PTSD. This hyperactivity contributes to heightened anxiety and arousal, making it difficult to fall asleep and stay asleep. Furthermore, dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, the body’s stress response system, plays a significant role.
Chronic stress associated with PTSD leads to elevated cortisol levels, disrupting the sleep-wake cycle. Neurotransmitter imbalances, particularly in serotonin and norepinephrine, further contribute to sleep disturbances. These physiological changes create a vicious cycle, where sleep deprivation worsens PTSD symptoms, leading to further sleep disruptions.
Impact of Sleep Deprivation on PTSD Symptoms
Sleep deprivation significantly exacerbates PTSD symptoms. Lack of sleep impairs cognitive function, making it harder to manage distressing memories and emotions. It also increases irritability, anxiety, and emotional reactivity, heightening the risk of experiencing flashbacks and nightmares. The impaired cognitive function also affects the ability to engage in effective coping strategies. Furthermore, sleep deprivation weakens the immune system, making individuals more vulnerable to illness, which can further compound their suffering.
In essence, sleep deprivation creates a cascade of negative consequences that worsen the overall impact of PTSD.
Comparison of Sleep Disorders in PTSD
| Type | Symptoms | Prevalence | Treatment Approaches |
|---|---|---|---|
| Insomnia | Difficulty falling asleep, staying asleep, or experiencing non-restorative sleep. | High; often the primary sleep complaint in PTSD. | Cognitive Behavioral Therapy for Insomnia (CBT-I), sleep hygiene education, medication (e.g., zolpidem, trazodone). |
| Nightmares | Vivid and disturbing dreams, often related to the traumatic event. | Very common; can significantly disrupt sleep and increase daytime anxiety. | Imagery Rehearsal Therapy (IRT), nightmare medication (e.g., prazosin). |
| Sleepwalking/Sleep Terrors | Episodes of walking or exhibiting frightening behaviors during sleep. | Less common than insomnia and nightmares, but can be distressing for both the individual and their family. | Addressing underlying PTSD symptoms, medication in severe cases. |
| Hyperarousal | Difficulty relaxing, frequent awakenings, and increased physiological arousal at night. | Common; contributes to insomnia and other sleep disturbances. | Relaxation techniques, CBT, medication (e.g., antidepressants). |
Therapeutic Interventions for Improving Sleep in PTSD
Improving sleep in individuals with PTSD requires a multifaceted approach, often combining therapeutic interventions and, in some cases, medication. The goal is to address both the underlying trauma-related symptoms and the resulting sleep disturbances. Effective treatment strategies aim to break the cycle of trauma-related nightmares, hyperarousal, and sleep disruption, leading to improved sleep quality and overall well-being.
Cognitive Behavioral Therapy for Insomnia (CBT-I) in PTSD
CBT-I is a highly effective treatment for insomnia, and its efficacy extends to individuals with PTSD. This therapy focuses on identifying and modifying unhelpful thoughts and behaviors that contribute to sleep problems. Techniques include stimulus control (creating a relaxing bedtime routine and using the bed only for sleep and sex), sleep restriction (gradually increasing time in bed based on actual sleep time to consolidate sleep), relaxation training, and cognitive restructuring (challenging negative thoughts and beliefs about sleep).
Studies consistently demonstrate that CBT-I significantly reduces insomnia symptoms in PTSD patients, leading to improvements in both sleep quality and daytime functioning. The success of CBT-I lies in its ability to empower individuals to manage their sleep independently, equipping them with long-term coping skills.
Pharmacological Interventions for Sleep in PTSD
Medication can be a valuable adjunct to therapy, particularly in the initial stages of treatment when sleep disturbance is severe. However, it’s crucial to understand that medication alone is rarely sufficient for long-term management of PTSD and sleep problems. Commonly prescribed medications include:
- Hypnotics: These medications induce sleep, but their long-term use can lead to dependence and tolerance. Examples include zolpidem (Ambien) and eszopiclone (Lunesta). Side effects may include daytime drowsiness, dizziness, and cognitive impairment.
- Antidepressants: Certain antidepressants, such as sertraline (Zoloft) and paroxetine (Paxil), are also effective in treating PTSD symptoms, including sleep disturbances. They work by regulating neurotransmitters in the brain, but can have side effects such as nausea, weight changes, and sexual dysfunction. These are often prescribed for longer-term management of PTSD, rather than solely for sleep.
- Prazosin: This medication is primarily used to treat hypertension, but it has also shown effectiveness in reducing nightmares in PTSD. Side effects are generally mild and include dizziness and lightheadedness.
It is essential that medication be prescribed and monitored by a healthcare professional experienced in treating PTSD.
Relaxation Techniques for Managing Sleep Problems Related to PTSD
Relaxation techniques can be powerful tools for managing the physiological arousal associated with PTSD and improving sleep. These techniques help to calm the nervous system and promote relaxation.
- Progressive Muscle Relaxation: This technique involves systematically tensing and releasing different muscle groups in the body. By focusing on the physical sensations of tension and release, individuals learn to identify and reduce muscle tension, which often contributes to sleep difficulties.
- Meditation and Mindfulness: Mindfulness meditation encourages focusing on the present moment without judgment, helping to quiet the mind and reduce racing thoughts that can interfere with sleep. Various meditation techniques, including guided meditations and body scans, can be particularly beneficial for PTSD.
Regular practice of these techniques is key to experiencing their benefits. These methods can be learned through self-help resources or with the guidance of a therapist.
Resources for Sleep Improvement in PTSD
Several resources offer support and guidance for improving sleep in individuals with PTSD. These resources can provide valuable information, tools, and techniques to help manage sleep problems.
- Books: “The PTSD Workbook” by Mary Beth Williams, “Overcoming Trauma Through EMDR” by Francine Shapiro.
- Websites: The National Center for PTSD website (ptsd.va.gov), The National Sleep Foundation website (sleepfoundation.org).
- Apps: Many meditation and mindfulness apps (such as Calm or Headspace) offer guided meditations specifically for sleep and stress reduction.
Stress and Anxiety Management Techniques
Stress, anxiety, and sleep disturbances are intricately linked. Chronic stress and anxiety activate the body’s stress response, leading to the release of hormones like cortisol. Elevated cortisol levels can interfere with sleep onset, maintain sleep, and lead to poor-quality sleep, characterized by frequent awakenings and difficulty returning to sleep. This disrupted sleep cycle, in turn, exacerbates stress and anxiety, creating a vicious cycle that negatively impacts both mental and physical health.
Addressing stress and anxiety is therefore crucial for improving sleep quality in individuals with PTSD.
Evidence-Based Stress Reduction Techniques, Sleep and PTSD management
Effective stress management involves a multi-pronged approach incorporating various techniques tailored to individual needs and preferences. The following techniques have demonstrated efficacy in reducing stress and improving sleep:
- Progressive Muscle Relaxation (PMR): This technique involves systematically tensing and releasing different muscle groups in the body. By focusing on physical sensations, individuals learn to identify and release muscle tension associated with stress and anxiety, promoting relaxation and sleep. A typical session involves tensing a muscle group for a few seconds, then releasing the tension and noticing the difference in sensation.
This is repeated for various muscle groups throughout the body, starting with the toes and working upwards.
- Diaphragmatic Breathing (Deep Breathing): Deep, slow breaths activate the parasympathetic nervous system, counteracting the effects of the stress response. This technique involves focusing on deep, abdominal breaths, allowing the belly to rise and fall with each inhalation and exhalation. Practicing diaphragmatic breathing regularly can significantly reduce heart rate and blood pressure, promoting relaxation and better sleep.
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and challenge negative thought patterns and beliefs contributing to stress and anxiety. By restructuring unhelpful thoughts and developing coping mechanisms, CBT helps individuals manage stress more effectively and improve sleep quality. This therapy often involves identifying triggers, practicing relaxation techniques, and developing problem-solving skills.
- Regular Exercise: Physical activity is a powerful stress reliever. Exercise releases endorphins, natural mood boosters, and improves sleep quality by regulating the body’s sleep-wake cycle. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Examples include brisk walking, jogging, swimming, or cycling.
- Yoga and Tai Chi: These mind-body practices combine physical postures, breathing techniques, and meditation to promote relaxation and reduce stress. Yoga and Tai Chi improve flexibility, strength, and balance while calming the nervous system, leading to improved sleep.
The Role of Mindfulness in Stress and Anxiety Management
Mindfulness involves paying attention to the present moment without judgment. Mindfulness practices, such as meditation and mindful breathing, help individuals become more aware of their thoughts, feelings, and bodily sensations, reducing the tendency to overreact to stressors. By cultivating present moment awareness, mindfulness helps individuals detach from anxious thoughts and worries, promoting relaxation and improving sleep quality. Mindful activities, like paying close attention to the sensation of a warm bath or the taste of food, can ground individuals in the present and interrupt cycles of rumination and anxiety.
A Sample Stress Management Plan
A comprehensive stress management plan should incorporate a combination of relaxation techniques and healthy lifestyle choices. This plan could include:
- Daily Mindfulness Practice: 10-15 minutes of daily meditation or mindful breathing exercises.
- Regular Exercise: At least 30 minutes of moderate-intensity exercise most days of the week.
- Progressive Muscle Relaxation: Practicing PMR before bedtime to promote relaxation and sleep.
- Healthy Diet: Limiting caffeine and alcohol intake, and ensuring a balanced diet rich in fruits, vegetables, and whole grains.
- Consistent Sleep Schedule: Maintaining a regular sleep-wake cycle by going to bed and waking up at the same time each day, even on weekends.
- Stress-Reducing Activities: Incorporating enjoyable activities into the daily routine, such as spending time in nature, listening to music, or engaging in hobbies.
Depression Support Resources and Strategies
Depression significantly impacts an individual’s well-being, often intertwining with sleep disorders and PTSD. Understanding available resources and strategies is crucial for effective management and recovery. Recognizing the signs and seeking appropriate support are vital steps in navigating this challenging condition.Depression, characterized by persistent sadness, loss of interest, and changes in sleep and appetite, requires a multifaceted approach to treatment.
Effective management involves a combination of self-help strategies, support networks, and professional intervention. Ignoring depression can lead to serious consequences, highlighting the importance of proactive engagement with available resources.
Types of Therapy Effective in Treating Depression
Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT) are two widely recognized and effective therapeutic approaches for depression. CBT focuses on identifying and modifying negative thought patterns and behaviors contributing to depressive symptoms. It equips individuals with practical skills to manage their thoughts and feelings more effectively. IPT, conversely, centers on improving interpersonal relationships and resolving conflicts that might exacerbate depressive episodes.
Both therapies involve structured sessions with a trained therapist and often incorporate homework assignments to reinforce learned skills. Other therapies, such as psychodynamic therapy and acceptance and commitment therapy (ACT), may also be beneficial depending on individual needs and preferences.
Depression Support Groups and Helplines
Accessing support networks can significantly improve the experience of managing depression. Support groups provide a safe space for individuals to share their experiences, connect with others facing similar challenges, and gain valuable insights from shared struggles and coping strategies. These groups often foster a sense of community and reduce feelings of isolation. Helplines offer immediate access to trained professionals who provide emotional support, guidance, and referrals to appropriate resources.
The anonymity and immediate accessibility offered by helplines are particularly beneficial for individuals who might hesitate to seek face-to-face support.
The Importance of Seeking Professional Help for Depression
While self-help strategies and support groups are valuable components of depression management, professional help is often essential for comprehensive treatment. A mental health professional, such as a psychiatrist, psychologist, or therapist, can conduct a thorough assessment, diagnose the condition accurately, and develop a personalized treatment plan. This plan may include medication, therapy, or a combination of both, tailored to the individual’s specific needs and circumstances.
Professional intervention helps ensure that individuals receive appropriate care and guidance, improving their chances of recovery and reducing the risk of relapse.
Resource Guide for Depression Support
Finding the right resources can be overwhelming. This guide provides a starting point for individuals seeking help.
- The National Institute of Mental Health (NIMH): Offers comprehensive information on depression, including symptoms, diagnosis, treatment options, and research findings. Website: [Insert NIMH website address]
- The Depression and Bipolar Support Alliance (DBSA): Provides peer support groups, educational resources, and advocacy for individuals affected by mood disorders. Website: [Insert DBSA website address]
- The National Alliance on Mental Illness (NAMI): Offers support groups, educational programs, and advocacy for individuals and families affected by mental illness. Website: [Insert NAMI website address]
- The Crisis Text Line: Provides free, 24/7 support via text message for individuals in crisis. Text HOME to 741741.
- The Suicide & Crisis Lifeline: Provides free and confidential support for people in distress. Dial or text 988.
Mindfulness Practices for PTSD and Sleep Improvement
Mindfulness practices offer a powerful approach to managing PTSD symptoms and improving sleep quality. By cultivating present moment awareness, individuals can learn to regulate their emotional responses, reduce hyperarousal, and promote relaxation, all crucial for overcoming the sleep disturbances often associated with PTSD. These techniques work by gently shifting focus away from intrusive thoughts and anxieties, creating space for calm and restorative rest.Mindfulness techniques, particularly meditation and body scan meditation, help to regulate the nervous system and promote relaxation by cultivating a state of focused attention.
This focused attention interrupts the cycle of negative thought patterns and physiological arousal often characteristic of PTSD. The practice encourages a shift from the sympathetic nervous system (fight-or-flight) to the parasympathetic nervous system (rest-and-digest), facilitating relaxation and better sleep.
Meditation for PTSD and Sleep
Meditation involves focusing your attention on a single point of reference, such as your breath, a mantra, or a visual image. This focused attention helps to quiet the mind and reduce racing thoughts, which are common in PTSD. Regular meditation practice can lead to increased self-awareness, emotional regulation, and improved sleep. Studies have shown that mindfulness meditation can significantly reduce PTSD symptoms, including nightmares and sleep disturbances.
For example, a study published in the Journal of Consulting and Clinical Psychology found that mindfulness-based interventions were effective in reducing PTSD symptoms in veterans.
Body Scan Meditation for PTSD and Sleep
Body scan meditation involves systematically bringing awareness to different parts of the body, noticing sensations without judgment. This practice helps to increase body awareness and reduce tension, which can be particularly helpful for individuals with PTSD who often experience heightened physical arousal. By focusing on physical sensations, individuals can learn to differentiate between genuine physical discomfort and the anxiety-related sensations often associated with PTSD.
This increased awareness can lead to a greater sense of control and a reduction in anxiety, promoting relaxation and better sleep. The process of systematically scanning the body helps to ground the individual in the present moment, reducing the tendency to dwell on past traumas or worry about the future.
Guided Meditation Script for Relaxation and Sleep
Find a comfortable position, either lying down or sitting upright. Close your eyes gently. Begin by noticing your breath, the natural rise and fall of your chest or abdomen. Don’t try to change your breath, simply observe it. Now, bring your attention to your body, starting with your toes.
Notice any sensations—tingling, warmth, coolness, pressure—without judgment. Simply acknowledge them. Slowly move your awareness up your body, noticing your feet, ankles, calves, knees, thighs, hips, abdomen, chest, back, shoulders, arms, hands, fingers, neck, face, and head. With each part of your body, acknowledge any sensations without judgment. Allow any tension to melt away with each exhale.
Continue to focus on your breath, feeling the calming rhythm. Repeat silently to yourself, “I am safe. I am peaceful. I am relaxed.” Let go of any worries or anxieties. Allow yourself to drift into a state of deep relaxation and peaceful sleep.
Mental Health Advocacy and Resources
Navigating the challenges of PTSD and other mental health conditions is significantly easier with the right support. This section highlights key organizations offering assistance and discusses the crucial role of advocacy in improving mental health services and reducing stigma. Understanding available resources and actively participating in advocacy efforts can empower individuals and communities to build a more supportive environment for those struggling with mental health.Accessing appropriate mental health care is paramount for recovery and well-being.
Many individuals face significant barriers, including financial constraints, lack of awareness about available services, and the persistent stigma associated with mental illness. Overcoming these obstacles requires a multifaceted approach involving both individual action and collective advocacy.
Key Organizations and Advocacy Groups
Several organizations provide invaluable support to individuals affected by PTSD and other mental health conditions. These groups offer a range of services, from direct support and counseling to advocacy and public awareness campaigns. Their work is vital in connecting individuals with resources and fostering a more understanding society.
- The National Center for PTSD (NCPTSD): The NCPTSD is a leading resource for information and support related to PTSD. They offer a wealth of educational materials, treatment guidelines, and links to local resources. Their website is a comprehensive starting point for anyone seeking information about PTSD.
- The Department of Veterans Affairs (VA): The VA provides comprehensive mental health services to veterans, including those suffering from PTSD. Their services range from individual therapy and group support to specialized treatment programs.
- The American Psychological Association (APA): The APA is a professional organization for psychologists, offering resources and information on various mental health conditions, including PTSD. They advocate for evidence-based treatments and promote mental health awareness.
- The National Alliance on Mental Illness (NAMI): NAMI is a grassroots organization dedicated to improving the lives of individuals and families affected by mental illness. They offer support groups, educational programs, and advocacy initiatives.
Reducing the Stigma Surrounding Mental Health
The stigma associated with mental health conditions remains a significant barrier to seeking help. Many individuals hesitate to disclose their struggles due to fear of judgment, discrimination, or social isolation. Open conversations, public awareness campaigns, and personal storytelling are crucial in challenging these negative perceptions.
“Mental health is as important as physical health, and seeking help is a sign of strength, not weakness.”
Strategies for Advocating for Better Mental Health Services
Advocating for improved mental health services involves various actions, from contacting elected officials to participating in community awareness events. Collective action amplifies individual voices, leading to meaningful policy changes and increased access to care.
- Contacting elected officials to express support for legislation promoting mental health services and funding.
- Participating in or organizing community events to raise awareness about mental health issues.
- Sharing personal stories to help destigmatize mental illness and encourage others to seek help.
- Supporting organizations that advocate for improved mental health care.
- Educating oneself and others about mental health conditions and available treatments.
Therapy and Counseling Options for PTSD
Post-traumatic stress disorder (PTSD) significantly impacts a person’s life, and effective treatment is crucial for recovery. Several therapeutic approaches have proven beneficial, each offering unique strategies to address the core symptoms of PTSD. Understanding these options and the role of a therapist is essential for individuals seeking help.Therapeutic approaches for PTSD aim to help individuals process traumatic memories, manage distressing symptoms, and regain a sense of control over their lives.
The choice of therapy often depends on individual needs, preferences, and the severity of symptoms. Collaboration between the individual and their therapist is key to developing a personalized treatment plan.
Trauma-Focused Cognitive Behavioral Therapy (CBT)
Trauma-focused CBT is a widely recognized and effective treatment for PTSD. This approach combines cognitive techniques, which challenge and modify negative thought patterns and beliefs related to the trauma, with behavioral techniques that help individuals gradually confront trauma-related memories and situations. The goal is to reduce avoidance behaviors, improve coping skills, and ultimately reduce the intensity of PTSD symptoms.
For example, a person with PTSD related to a car accident might use CBT to challenge their fear of driving by gradually increasing exposure to driving situations, starting with short trips in a safe environment and progressively working up to longer drives on busier roads. Simultaneously, they would work on cognitive restructuring to challenge unhelpful thoughts such as “I’m never safe driving” and replace them with more balanced and realistic ones.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR therapy is another evidence-based treatment for PTSD. It involves bilateral stimulation, often through eye movements, while the individual focuses on the traumatic memory. This process is thought to help the brain process the traumatic memory more effectively, reducing its emotional impact. While the exact mechanism is still under research, EMDR is believed to facilitate the integration of traumatic memories into a person’s overall life narrative, thereby reducing the intensity of intrusive thoughts and emotional distress.
A person suffering from PTSD after a violent robbery, for instance, might use EMDR to process the memory of the event, reducing the vividness and emotional charge associated with it.
The Role of a Therapist in PTSD Treatment and Recovery
The therapist plays a vital role in guiding the individual through the PTSD treatment process. They provide a safe and supportive environment, helping the individual to explore their trauma, develop coping mechanisms, and process their emotions. Therapists create a therapeutic alliance based on trust and understanding, which is crucial for successful treatment. Beyond specific techniques, therapists offer ongoing support, encouragement, and education about PTSD, empowering individuals to take an active role in their recovery.
They also help identify and address any co-occurring conditions such as depression or anxiety, often tailoring treatment to the individual’s unique circumstances and needs.
Benefits of Group Therapy for Individuals with PTSD
Group therapy offers a unique setting for individuals with PTSD to connect with others who share similar experiences. This shared experience can foster a sense of validation, reduce feelings of isolation, and promote mutual support. Group therapy provides a space for learning from others’ coping strategies, receiving peer feedback, and practicing social skills in a safe environment. The group dynamic itself can be therapeutic, fostering a sense of community and belonging that can be particularly beneficial for individuals struggling with the isolation often associated with PTSD.
For example, a group therapy setting might allow individuals to share their experiences of nightmares or flashbacks, gaining comfort from knowing they are not alone and learning coping mechanisms from others.
Ultimately, achieving restful sleep is a cornerstone of PTSD management and overall recovery. By implementing the sleep hygiene strategies, therapeutic interventions, and stress management techniques discussed, individuals with PTSD can break the cycle of sleep disruption and symptom exacerbation. Remember, seeking professional help is paramount. A collaborative approach involving therapists, healthcare providers, and supportive loved ones can significantly improve sleep quality and lead to a more fulfilling and peaceful life.
Prioritizing self-care, building resilience, and accessing available resources are essential steps toward reclaiming control and experiencing a better quality of life.
Common Queries: Sleep And PTSD Management
What are the long-term effects of untreated sleep problems in individuals with PTSD?
Untreated sleep problems can lead to chronic fatigue, increased PTSD symptom severity, impaired cognitive function, weakened immune system, and a higher risk of developing other mental health conditions.
Can I use over-the-counter sleep aids for PTSD-related insomnia?
While some over-the-counter sleep aids might provide temporary relief, they are not a long-term solution and may have interactions with other medications. Consult a doctor before using any sleep aids, especially if you are taking other medications.
How can family members support someone with PTSD and sleep difficulties?
Family members can provide emotional support, encourage adherence to sleep hygiene practices, create a calm and supportive home environment, and learn about PTSD and its impact on sleep to better understand the challenges faced.
Are there specific types of therapy particularly effective for addressing sleep problems in PTSD?
Cognitive Behavioral Therapy for Insomnia (CBT-I) has shown significant effectiveness in treating insomnia related to PTSD. Other therapies, such as trauma-focused CBT and EMDR, can also indirectly improve sleep by addressing the underlying trauma.



