How to Help Someone with Depression
How to help someone with depression is a question many face. Understanding the nuances of depression, from recognizing its various symptoms and manifestations across different age groups to effectively communicating support, is crucial. This guide explores practical strategies for offering help, managing stress and anxiety, utilizing available resources, and promoting long-term well-being for both the individual struggling with depression and those supporting them.
We’ll delve into effective communication techniques, stress-reduction methods, and the importance of seeking professional help. We’ll also examine the role of mindfulness, building resilience, and fostering a supportive environment, including the workplace. The aim is to provide a comprehensive and compassionate approach to assisting someone navigating the challenges of depression.
Understanding Depression: How To Help Someone With Depression
Depression is a common and serious mood disorder that can significantly impact a person’s life. It’s characterized by persistent sadness and loss of interest in activities, causing significant impairment in daily functioning. Understanding its various forms and manifestations is crucial for effective support.
Common Signs and Symptoms of Depression, How to help someone with depression
Depression presents differently in individuals, but common signs and symptoms include persistent sadness or low mood, loss of interest or pleasure in activities once enjoyed (anhedonia), changes in appetite or weight (either significant weight loss or gain), sleep disturbances (insomnia or hypersomnia), fatigue or loss of energy, feelings of worthlessness or excessive guilt, difficulty concentrating, indecisiveness, and recurrent thoughts of death or suicide.
The severity and combination of these symptoms vary.
Types of Depression and Their Characteristics
Several types of depression exist, each with unique characteristics. Major Depressive Disorder (MDD), often called clinical depression, is characterized by a persistent low mood lasting at least two weeks, accompanied by other symptoms impacting daily life. Persistent Depressive Disorder (PDD), formerly known as dysthymia, involves a less intense but more chronic low mood lasting at least two years. Other types include postpartum depression (occurring after childbirth), seasonal affective disorder (SAD, related to changes in seasons), and bipolar disorder (characterized by alternating periods of depression and mania).
The specific symptoms and their intensity differ across these types.
Manifestations of Depression Across Age Groups
Depression manifests differently across age groups. In children and adolescents, it might present as irritability, difficulty concentrating in school, social withdrawal, or changes in behavior. Young adults might experience academic or occupational difficulties, relationship problems, or substance abuse. In older adults, symptoms may include physical complaints, memory problems, or social isolation. Accurate diagnosis requires considering the individual’s developmental stage and life context.
Comparison of Major Depressive Disorder and Persistent Depressive Disorder
| Feature | Major Depressive Disorder (MDD) | Persistent Depressive Disorder (PDD) | Difference Summary |
|---|---|---|---|
| Duration | At least two weeks | At least two years | MDD is episodic, PDD is chronic |
| Severity | Symptoms are severe enough to cause significant impairment in daily life | Symptoms are less severe than MDD but persistent | MDD involves more intense symptoms |
| Symptom Profile | May include all common depressive symptoms | Typically includes a persistent low mood with fewer intense episodes | MDD has a broader range of potential symptoms |
| Treatment | Often requires medication and/or therapy | Usually requires long-term therapy and may involve medication | Both require treatment, but PDD often necessitates a longer-term approach |
Approaching Someone with Depression
Approaching someone you suspect is struggling with depression requires sensitivity, empathy, and a genuine desire to help. It’s crucial to remember that there’s no one-size-fits-all approach, and your actions should be guided by the individual’s comfort level and your existing relationship. Open communication and a non-judgmental attitude are paramount.Effective communication strategies are vital when talking to someone who may be depressed.
Avoid using clichés or minimizing their experience. Instead, focus on active listening and creating a safe space for them to express their feelings without interruption or judgment. Your goal is to show them you care and are there to support them, not to offer solutions or unsolicited advice.
Active Listening and Empathetic Responses
Active listening involves fully concentrating on what the person is saying, both verbally and nonverbally. This includes paying attention to their tone of voice, body language, and emotional cues. Empathetic responses demonstrate understanding and validation of their feelings. For example, instead of saying “Just snap out of it,” you might say, “It sounds like you’re going through a really tough time right now.
I’m here to listen if you want to talk about it.” Reflecting their emotions (“That sounds incredibly frustrating”) and validating their experience (“It’s understandable that you feel this way”) can help them feel heard and understood.
Offering Support Without Minimizing Feelings
Offering support means being present and available for the person without trying to fix their problems. Avoid phrases that diminish their feelings, such as “You’re too young to be depressed” or “Things could be worse.” Instead, focus on validating their experience and offering practical assistance where appropriate. This could include helping with daily tasks, accompanying them to appointments, or simply spending time with them.
Remember, your role is to be a supportive presence, not a therapist.
Steps to Initiate a Conversation About Depression
The following flowchart Artikels a suggested approach for initiating a conversation about depression. It emphasizes building trust and creating a safe space before directly addressing the issue.
Flowchart: Initiating a Conversation About Depression
Step 1: Choose the Right Time and Place
-Find a private, quiet setting where you can talk comfortably without interruptions. Ensure the person feels safe and relaxed.
Step 2: Express Your Concern
-Begin by expressing your concern for their well-being, using phrases like, “I’ve noticed you haven’t been yourself lately, and I’m worried about you.” Avoid accusations or judgment.
Step 3: Listen Actively and Empathetically
-Let them share their feelings without interruption. Use active listening techniques, such as reflecting their emotions and validating their experience.
Step 4: Offer Support and Encouragement
-Let them know you’re there for them and offer practical support. Encourage them to seek professional help if needed, but avoid pressuring them.
Step 5: Suggest Professional Help
-Gently suggest that they consider seeking professional help from a therapist or counselor. Offer to help them find resources or accompany them to appointments.
Step 6: Maintain Consistent Support
-Let them know you’re there for them in the long term. Continue to offer support and encouragement, even if they don’t immediately seek professional help.
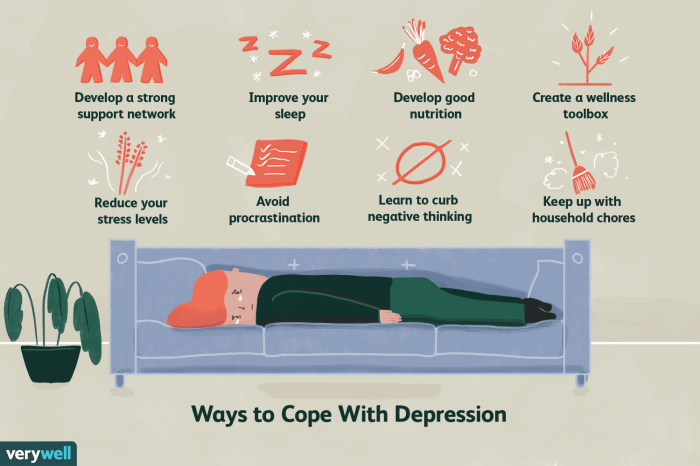
Helping someone through depression requires patience, understanding, and a commitment to supporting their journey toward recovery. While this guide offers valuable insights and practical strategies, remember that each individual’s experience is unique. Encouraging professional help, fostering open communication, and practicing self-care are key elements in navigating this complex issue. By combining empathy, knowledge, and the utilization of available resources, we can create a supportive environment where healing and recovery are possible.
Top FAQs
What if the person refuses help?
Respect their decision, but continue to express your concern and availability. Offer support without pressure, and suggest they reconsider when they are ready.
How can I avoid burnout while supporting someone with depression?
Prioritize your own well-being. Engage in self-care activities, set boundaries, and seek support from friends, family, or a therapist.
What are some early warning signs of depression I should look for?
Persistent sadness, loss of interest in activities, changes in sleep or appetite, fatigue, feelings of worthlessness, and difficulty concentrating are common signs.
Is it okay to talk about suicide with someone who might be depressed?
Yes, it’s crucial. Ask directly if they are having suicidal thoughts and encourage them to seek professional help immediately. Don’t be afraid to seek help from a crisis hotline or emergency services.



